Anne Lambie interview 2020
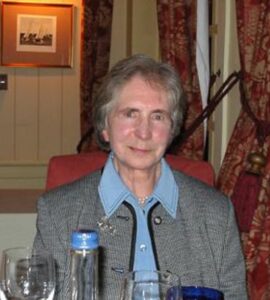 Anne Lambie was one of the first nephrologists in Edinburgh, involved in the first dialysis for acute renal failure in 1959, and leading the acute service over the next two decades. Edinburgh was the 6th or 7th unit to get a dialysis machine. She was closely involved in the first successful UK kidney transplant, and one of the UK’s pioneer transplant programmes. She is remembered as a memorably clear teacher and sympathetic trainer, respected for her personal and detailed patient care. She was also a pioneer as one of a handful of female consultants in teaching hospitals at the time.
Anne Lambie was one of the first nephrologists in Edinburgh, involved in the first dialysis for acute renal failure in 1959, and leading the acute service over the next two decades. Edinburgh was the 6th or 7th unit to get a dialysis machine. She was closely involved in the first successful UK kidney transplant, and one of the UK’s pioneer transplant programmes. She is remembered as a memorably clear teacher and sympathetic trainer, respected for her personal and detailed patient care. She was also a pioneer as one of a handful of female consultants in teaching hospitals at the time.
The recording is in 3 parts. Each has links to the audio, and to the appropriate part of the transcript, which is shown in full further down the page. You can also download the entire transcript (pdf, 120 kb).
Contents
Contents
RECORDING 1 10 mins. Listen to audio (in new tab) | Jump to transcript
- Starting Medical school aged 16 in 1945
- Endocrinology and general medicine. Addison’s disease before and after 1950
- Research in Boston
RECORDING 2 44 mins. Listen to audio (in new tab) | Jump to transcript
- Research in Boston, 1954
- Interest in nephrology. Seeing dialysis at the Brigham hospital
- Return to Edinburgh as senior registrar in 1956; starting a research lab
- Experiences with dialysis for ARF. Teamwork.
- Hepatitis hits Edinburgh
- Transplantation, and the beginnings of dialysis for CRF
- Greatest changes in practice
RECORDING 3 17 mins. Listen to audio (in new tab) | Jump to transcript
- Peritoneal dialysis (00.10 chapter 1)
- Undergraduate teaching (04.17 chapter 2)
- Looking back on the route taken, and some professional advice (11.50 chapter 3)
Transcript
N: So I thought we might start out by just talking a little bit about how you got into medicine and your early experiences at medical school in what must have been a minority of women.
A: I decided that I wanted to be a doctor very early, there were a number of members of my family who were medically qualified. And at that point, I wasn’t really quite sure what sort of doctor I wanted to be.
I applied for admission to Edinburgh when I was in the sixth form at school, doing my higher school certificate and was told that although I was relatively young, it would be wise to apply that year because the following year, they were anticipating a surge of ex-service people coming back to do medicine. So I came up to Edinburgh in the autumn of 1945. And at that time, the women were taught separately for anatomy in the same dissecting room, but there were certain tables set aside for the girls and the staff who taught them, among them Dr. Barrett and Miss McKay were ladies. Apart from that, the thing I found most difficult, I think, was coming into a large mixed class, having been at an all-girls school. By the time I was a medical student, the presence of women in medicine, of course, was perfectly established. The only thing was a great many people in my year, girls in my year, were actually the daughters of doctors and, in a sense, had a job prepared for them ahead.
N: And how many were there in your year?
A: About 20% of 200.
N: And you were very young, you’re saying, how old were you?
A: I wasn’t quite 17, I was actually the youngest in the year. I found the first year a little difficult. Mostly because I found dissecting a little unpleasant and I rather dithered during the first 12 months as to whether to try and switch to pure science. And then I discovered that there were a wide variety of openings to someone with a medical degree and decided that I should certainly continue.
N: You ended up in a specialty which, while it’s got a lot of science also has a huge amount of patient contact. What brought about that change?
A: Well, when I qualified I eventually, a year later, got the job I wanted with Professor Dunlop as an SHO (Senior House Officer). And I did two years of pure clinical medicine with special interest in endocrinology. And then at that point, it was suggested that a couple of years in the States would be a good thing. And I went off to join Arnold Relman and Bill Schwartz in Boston. That was two years of pure research, practically no clinical work.
N: Can I just flip back to Derrick Dunlop, who was a tremendously well-regarded physician, wasn’t he? Quite influential. What was it about his personality or his patients that attracted you?
A: He was a brilliant teacher. He was involved in endocrinology, which was a subject I thought I could understand a bit about. It was a prestigious job. And I was aware that if I was going to remain in hospital medicine, I had to have as many things in my favour as possible.
N: So who were the patients at the time? What was wrong with them?
A: All the physicians in the Royal Infirmary at that time were general physicians. In other words, they all took [admitted general medical emergencies] once a week, an influx of people with a variety of a variety of conditions. So there was general medicine. The specialist cases who came in were people with pituitary, adrenal, thyroid disease and diabetes. But most of them were actually in a special little metabolic ward. Although at that particular time, there was very little research going on.
N: You mentioned to me previously, the experience of looking after patients with Addison’s disease in the late 1940s, before prednisone had come along.
A: Yes, it would be actually when I was a third or fourth year student. At that stage cortisone was not available. By the time I qualified, it was available, but under very severe restrictions. Before it became available, one treated patients with Addisonian crisis by treating the underlying cause, by treating them with restoration of the extracellular volume, with usually glucose saline, correcting the carbohydrate metabolism as well. And with implants of desoxy-corticosterone acetate, which was essentially a mineralocorticoid.
N: And then was it fairly transformed when you came back as an SHO?
A: It was very much transformed. It ceased to be a likely death sentence.
N: Should we switch to your time in Boston?
A: Yes. Relman and Schwartz were part of a coterie of young men who had been trained by John Peters in Yale, who was an outstanding clinician and scientist. They were also part of the salt and water club, of the eastern seaboard of the States. And I think, as I said in my article, those of us who were working with them in the 1950s rather liked to regard ourselves as Peters’ great intellectual grandchildren. I think the main things I learned there was how to set up and run a laboratory, which I had no previous experience of. And then, for the first time, I had experience in research in animals, mostly rats, and we were looking at transport of ions into cells, in a very old fashioned and primitive fashion. But we also saw cases of acute electrolyte disturbance and renal problems on the wards. And I found that very interesting, and that was really where my first experience of nephrology came. Renal biopsy had just been developed at that time. Neither Relman nor Schwartz were prepared to do needle biopsies because they considered it was potentially dangerous, so patients who had a very good reason to have a renal biopsy had an open operative biopsy done.
- Research in Boston, 1954
- Interest in nephrology. Seeing dialysis at the Brigham hospital
- Return to Edinburgh as senior registrar in 1956; starting a research lab with Jim Robson
- Experiences with dialysis
- Hepatitis
- Transplantation, and the beginnings of dialysis for CRF
- Greatest changes
A: Going back to my last two years at school, we had Dr. Guthrie, who had just finished doing a PhD in physical chemistry.
N: You were talking about Boston, and the salt and water club, and being disciples of Peters. And you’d seen some patients on the wards and that began to get you interested in nephrology.
A: And I also became very interested in sodium and potassium transport in the kidney. Something which I had already actually done a little bit about because Andrew Wilkinson, when he was a senior registrar with Learmonth, was doing some research. And I helped him a little by doing blood pressures. And he talked to me quite a lot about water and electrolytes and the metabolic response to surgery.
N: And what was the key research that you did while you were in Boston?
A: My key research was looking at the transport of sodium and potassium into cells, using rubidium as a marker. In retrospect, it wasn’t very good research because of course rubidium poisoned the channels. I was also involved in assisting Arthur Kunin, who subsequently became Professor of Medicine in Vermont, with studies on the excretion of potassium. And I was involved in balance studies on one of the first cases of Conn’s syndrome, which was very interesting indeed. And also a lesson in how to do balances. I got involved as an extra pair of hands to cover weekends when Bill Schwartz was doing his original work on the syndrome of inappropriate ADH, which was extremely interesting. Those were the main things. We also got a chance to go over to the Brigham and see what they were doing there.
They were doing a certain amount of haemodialysis using the Kolff-Brigham machine. Also Hume had just started doing transplants. And as I say, we saw some renal biopsy work but it was done by operative biopsy.
N: So you saw haemodialysis when you were there primarily as a research attachment.
A: Yes, I just saw it. I mean, it was a fleeting visit to the Brigham.
N: You mentioned being called to renal consults during your time there. And I wonder what sort of abnormalities were you called to see – was that acute renal failure, or other issues?
A: The ones I remember were people with, there weren’t many. There were more electrolyte disturbances. People with severe pyelonephritis. One or two people with proteinuria almost certainly had glomerulonephritis before they started doing biopsies.
N: Was it called glomerulonephritis then?
A: Yes. The people we saw on the wards were mostly salt and water problems.
N: And when you came back to the UK, back to Edinburgh what did you return to?
A: I came back to Derrick Dunlop’s wards. I came back to being the senior registrar in charge of the metabolic ward with responsibilities on waiting day [reviewing and admitting acute unselected medical patients] in the general wards.
N: Which year are we in now?
A: We’re in late 1956. And at that point during the last couple of months I was in Boston, CP Stewart visited us. He was a professor of clinical chemistry in the Edinburgh Royal Infirmary. He was a very kind, helpful man. The interesting thing was that in Europe, as I discovered later, he was greatly admired as the father of clinical chemistry. He was very much ‘prophet without honour’ in his own country. Anyhow, CP came to Boston to see Relman, Schwartz and Peters and one or two other people. And when he was visiting Relman I went along for coffee. And when he was leaving, he said, ‘Well, when you come home, let me know. And I’ll try and provide you with the laboratory facilities you need’. So, in that way, I got involved with James Robson, who was then a senior registrar in Sir Stanley Davidson’s ward. Just before I came home, we had a journal club, and we had been reading with Relman the work on water excretion. And the concept of TCH20 and free water clearance, and I came home with the idea that it would be interesting to look at this in patients with Addison’s disease, and because one knew that they couldn’t excrete water, one wondered whether they also couldn’t concentrate. Also, I had in mind the idea that it would be interesting to look at diuretics. And I found that JSR (James Robson) had the same idea about steroids. So we decided to collaborate and CP provided laboratory facilities. He provided us serially with an osmometer, a small flame photometer, and finally a Van Slyke machine, all of which I had actually learned to use in the States. And that was where the research programme really started.
N: What did you pick up? You mentioned two areas there. The first was water clearance in Addison’s and the second was diuretics, of which there weren’t so many then.
A: We both thought independently, it would be interesting to know what actually happened to pure water excretion when you give a diuretic.
N: And what would the diuretics be that you were testing in 1956? You mentioned mercurials.
A: I think mercurials were the first we looked at, and of course that’s interesting because they act on the loop. We incorporated that into an exercise in clinical pharmacology for the pharmacology students. So that was really where the research in renal and electrolytes started.
N: And at some point, during these first couple of years back, people started talking about whether dialysis was something that we should be doing in Britain. Is that right?
A: Yes, that I think was actually 1958. I’d been back for two years. And Dr Gilchrist, who was a cardiologist had been to symposium in Sweden and had met Nils Alwall. and was very impressed with what he was doing. Apparently, he stood up in the physicians meeting, which we of course, weren’t at and said, ‘I’m going to get an artificial kidney for this hospital’, which was very Gilchrist!
N: Were you involved in the group looking at that?
A: No. They said it was a job for young men and they meant men, which I think was very unfair, they asked Robson and Hugh Dudley to go. They had both been working on water and electrolyte subjects and also on the metabolic response to surgery.
N: Did either of them have very much experience of managing acute renal failure then?
A: No, no one in Edinburgh had. I mean, as far as we were concerned, it was something that had happened in the Blitz, and had been reported, and by and large had been treated with the special diet.
N: But not on your ward and not on Jim Robson’s service either.
A: No, no, I don’t think either of us had seen a case of acute renal failure.
N: And yet they must have been there.
A: Yes, they must have been, they must have died quietly in the surgical ward. And what Robson and CP Stewart had done before I went to the States was start to treat patients with chronic renal failure by conservative means, and I was very impressed by the degree of improvement you could get.
N: What lines of treatment were they following?
A: Well essentially, they were rehydrating them – re-expanding the extracellular fluid volume with a bit of saline and treating metabolic acidosis with bicarbonate capsules, reducing the protein intake, and trying to encourage a high non-protein calorie intake. But it was a revelation to me how much the patients improved.
N: This sounds very much like the line of treatment in Addis’s book [Glomerular Nephritis (1949)]. So they were looking after chronic renal failure at that point but had very little experience of acute renal failure. Fascinating, isn’t it?
A: I didn’t really see a case of acute renal failure at that time in Edinburgh. I saw a case of acute renal failure [acute kidney injury] in Boston, in a young woman with Staphylococcal pneumonia. In whom we simply restricted fluids for a day or two, until her pneumonia was treated and she recovered. But she never became significantly uraemic.
N: So, to skip over surveying what kind of machine to get, and the Dudley-Robson report, and the purchasing, a machine arrived, and I think you did become involved with that?
A: Yes, at that point it was suggested that I should join the party. In fact, just before the machine arrived, Dudley moved to Aberdeen and I joined in partnership with Jim Robson when we went down to Leeds with a patient to see what was happening there [elsewhere Anne described this as being in a small aeroplane with the patient, in dense fog]. That was very interesting, because of course, the whole emphasis was bigger and more powerful machines. Particularly for the hypermetabolic patient.
N: So they had a machine like the one in Boston – a rotating drum device with a huge capacity. And do you remember the first patient who came in and needed dialysis in Edinburgh?
A: Yes. I mean, we were very lucky, because the first patient was eminently treatable. We got a young man who had biliary sepsis and an impacted gall stone, and an acutely infected gall bladder, and bacteraemia, who was essentially anuric. And we treated him with a single dialysis, started him on an antibiotic, the surgeons then drained his gallbladder, his urea continued to rise, and he was dialyzed a second time. And then after that his renal function recovered steadily.
N: And what was the process of putting a patient on dialysis like then?
A: Well, it was rather frightening because you we didn’t really know what was going to happen. And there wasn’t anything much in the literature. By and large, you had to follow what people who had units in England had told you and use what knowledge of physiology you had.
There were no failsafe devices, and with the Kolff-Travenol machine, you could remove fluid by putting a clamp with varying degrees of tightness on the outflow lines. And the only way you could estimate how much the patient had lost in the way of extracellular fluid was by repeated weighing. We had a weighing machine that the bed sat on, but it wasn’t an accurate procedure. So there was a certain amount of guessing there. We estimated the blood chemistry every two hours and changed the bath [the tank of dialysis fluid that the drum rotated in] every two hours.
N: So how many people did these? How many staff were involved in each treatment?
A: One staff nurse, Robson and myself. My husband [Howard Davies] doing the clotting. John Cowie in the lab, possibly a second technician.
N: And how long was each dialysis?
A: The actual dialysis would be six hours, unless it was for poisons, in which case it was eight or nine hours. The setting up probably took an hour. And there was sometimes a little bit of biochemistry to do after the thing had finished. So you’re probably talking about nine hours or so. It was very staff intensive.
N: And who was connecting the circulation to the machine,
A: One of the surgeons, Ian Sinclair. And initially, of course, it was a matter of cutting down every time. And that could take a variable amount of time, depending on how collapsed the patient was.
N: And then, at some point, the antecedent of what we later recognised as the conventional Scribner shunt came along to help.
A: Yes, it was a bit difficult, but eventually, it evolved into a simple tube that you just disconnected the artery part from the vein.
N: I think someone constructed these themselves in Edinburgh, one of those early shunts out of Teflon?
A: Yes I think it was the medical physicists did that.
N: Anne, later you seemed to assume administrative control over the treatment of acute renal failure by dialysis and wrote them all up. Is that right?
A: No, we never wrote the complete series up.
N: Perhaps I’m just remembering seeing the recordings in your book.
A: The interesting thing about acute renal failure was the way it changed over the years. And looking back, I realised how we’d really done pretty well keeping the mortality steady, in fact, getting a little improvement in the mortality. Because at the beginning, the cases were very straightforward. You were dealing with things like transfusion reaction, postpartum haemorrhage, the odd surgical case, like the very first one.
And then as things went on, it became more complicated. We started treating people who had much more severe sepsis or shock, because in the early days, they didn’t survive long enough to get to us. And then, there was a period, when we began to treat people with haematological problems like haemolytic uremic syndrome and DIC, where the outlook wasn’t so good.
And then open heart surgery. And that was quite funny, because I think in the early phase of open heart surgery, we had about nine or ten cases in the year. And I remember Mr. Logan saying, of course, it’s only a very small proportion of the ones we do. And of course I said this was a very high proportion of the severe cases we dialyse.
Despite that, and in spite of the fact that we were treating a lot of people with combined renal and respiratory failure, the mortality rate actually fell just a little. somewhere I have a … (refers to book) there was one in 1987, there was one in for 1988. That was renal, and respiratory.
N: So just as you described, these are getting much more complicated. Interestingly, this is the 1980s now and there’s only one obstetric example. Was that something that was dying down by then?
A: It was. Although we had a number of very bizarre cases, I can’t remember the date. But we had three cases, two from Glasgow, and one locally were patients who did not seem to have had any particular obstetric problems develop partial cortical necrosis. We never understood why that happened.
N: What happened to those patients?
A: They went on to chronic dialysis.
N: Which was available by then. So for quite a while there was only dialysis for acute renal failure?
A: Chronic dialysis started in 1964 when one of the large, refrigerated tanks that was in use in the States was purchased, and a small number of patients were treated. The dialysis was very long, about eight or nine hours. And at that point, it became obvious that one had to have a team of nurses which of course also facilitated the management of acute renal failure. So that was when chronic dialysis started.
N: Was that controversial?
A: Yes, there was a certain amount of controversy about that among the other physicians, whether this was a sensible or a good thing to do, particularly when it was involving so much resource. A few years later, we got automatic dialysis machines and were able to treat more patients for shorter periods.
N: Were you very much involved in that programme?
A: I was less involved in chronic renal failure. Acute renal failure was always my main major interest. I was involved to the extent that I obviously did a ward round and checked up on things. But I was never involved in any of the research to any extent.
N: This must have been a tremendously exciting and sometimes frightening period, with all this very new technology about, and debate about resource allocation.
A: Yes, that was difficult. Initially, we were really only dialysing young people on chronic dialysis. And one was terribly aware that it was a partial solution, that there was still a lot of things going wrong, like hyperparathyroidism, and also that it was still a pretty restricted life for the patients. As far as the general public were concerned, people were alive, who would have been dead. And therefore it was a tremendous thing.
N: Was there a debate about the relative position of transplantation at that time?
A: There was a lot of discussion. That was interesting, because at the [first] International Congress of Nephrology at Evian in 1960 the general feeling was, that transplant was really a very much better solution. By the time of the next Congress, it was, what, three years later in Prague, dialysis was much more accepted, and people were a lot more enthusiastic about it.
N: And, of course, in a bit of a blow to development in Edinburgh, in 1969, the nice new unit opened, but that was the year that hepatitis was first encountered.
A: That was really very frightening. Because, as you already know, there were a number of staff deaths, and quite a lot of patient deaths. And eventually, the problem was solved by the bacteriologist because there was a little monitor on the venous return side of the equipment into which blood passed during dialysis, and obviously, left traces. And it wasn’t changed because it was part of the machine. And Ralph Tonkin found that this was the way that it was being spread around. By that time, there had been quite a large number of cases. And of course, it involved the closure of the unit, until all these people had been transferred either to home dialysis or to a small special ward. So the programme effectively ceased for a little over a year.
N: You must have known some of the staff members who died or were affected by this.
A: Yes, they were both young, they were young surgeons. They had been involved in the operation on the index case. And there were a number of technicians who died who had been handling the blood.
N: What was the effect of all this on the way that both people inside the renal unit felt and operated, and on the attitudes of the rest of the hospital?
A: Some people in the rest of the hospital thought that the programme should come to an end. Understandably. The unit was marvellous and that was mainly due to our Senior Sister who had a tremendous capacity for keeping cool and keeping the morale of the nurses up. She subsequently got the MBE which was very well deserved. I think we just went on. I remember having to assist to stop nasal bleeding in a patient with hepatitis. There were just the three of us – myself, an ENT surgeon, and one of the nurses. Of course, he was pouring blood. We all had protective suits and whatnot. But that was quite scary. But Sister Harbison was splendid.
N: Did it impact on nurses and doctors coming to work on the unit?
A: I think the registrar staff didn’t turn over. It certainly didn’t stop SHOs coming.
We were in a way lucky because we were already taking precautions with gowns and gloves before the thing happened. The reason being that a year before one of the senior technicians in clinical chemistry developed jaundice. And we thought that this might possibly be hepatitis, which was already rampant in Manchester. So we went on to precautions at that point. The poor chap actually had a cousin who was the head of […]. But it might have been worse if we hadn’t done that.
N: I wasn’t aware of that bit of history. That’s fascinating. And so the unit got through that. That must have been one of the worst experiences, but maybe you’d had others.
A: No, that was very nasty. I think it probably was the worst experience.
N: Do you have a best experience? It must have been very exciting when your first patients on dialysis recovered, who seemed fated to die without it.
A: Yes. Yes, that was that really was exciting.
N: There weren’t very many units in the UK at that time. But there were a few and you were very closely in touch with what was going on the others?
A: The Renal Association had changed a bit and had become almost a place where people swapped dialysis experience. Perhaps just temporarily. So we were in touch. Then we were certainly in touch with Stanley Shaldon. With the Glasgow people of course; Bill Stewart in Dundee … I can’t remember the name of the chap in Manchester …
N: And at some point, Anne, and again, you weren’t too involved in chronic renal failure, but at some point, the mood in the country changed. And it was felt that dialysis was right to expand.
A: And then I think we went rather too far. In that, after I retired, Robin [Winney] was having to deal with patients brought in twice a week from nursing homes, who were not really well enough.
N: The pendulum has probably come back a bit in that chronic dialysis is discussed more realistically, I think. But it does give you a different kind of challenge.
N: The early days of renal units that you described, when it wasn’t clear whether dialysis was a long-term option, or whether transplantation was better. What was that like for the patients?
A: I think at that point, the general public didn’t know a great deal about it. I think from the very beginning, patients thought it would be nice to have a transplanted kidney. But of course, in the early 1960s immunosuppression wasn’t as satisfactory. And unless you had a twin, there wasn’t really a great deal of hope.
N: Were you involved in looking after those early transplant patients in Edinburgh? (Yes) Some of those must have started out with a lot of hope and ended up rather sadly.
A: Yes, there was one very sad one. The first lady, I think, to get a cadaver kidney who went down to the Western for whole body radiation and came back and had the kidney transplanted and died of overwhelming infection.
And then, of course, I think it was just after that we had this special unit built for the transplant patients.
N: With its bridge across to radiotherapy?
A: No, that was the one at the Western. There was a special one at the Royal first, where there was simply a set up where the patient was in the inner room. There was an outer room with showering facilities. And there was a clean and a dirty corridor. And in the dirty corridor, the medical physicists set up equipment so that we could talk to the nurses in the room. And they could pass out blood samples in the clean corridor; clean dressings, medicines, and what not went in. And that was helpful. But in fact, it was really only when they got the immunosuppression sorted out that it made a difference.
N: I think Edinburgh used azathioprine very early.
A: I think that’s right. And also anti-lymphocytic serum.
N: And there was a patient [name] who I think was transplanted in the mid 1960s, after a period of acute dialysis. She’s certainly our longest term survivor.
A: Yes, I’ve been in and spoken to her, I remember that.
N: Did you know her? in her early days, she was only about eight or 10.
A: Yes, yes, I know, in as much as I saw her when I was going around the medical renal unit
N: It’s astonishing, isn’t it, how some people through a mixture of luck and presumably either good personality or good genes managed to survive for decades?
I wonder whether you have any thoughts about what are the characteristics of these people who are able to manage this situation for a lifetime?
A: I think support at home was very important. And I think also they were people who were prepared to do what they were advised to do. I don’t know about genes; it would be interesting to know whether they came from families where people lived to a good old age.
N: You mentioned that when you studied diuretics, there were hardly any available. In fact, I think some of your work was based on mercurial diuretics and acetazolamide was possibly one of the others. And that just reinforces the limited drug range, back in those early days. So I wonder if you remember what, what the typical blood pressures of people with kidney failure was?
A: High! Systolic and diastolic. And the drugs available for that were not very helpful.
N: So the survivors must have had some resistance to that. Do you remember, apart from dialysis, any other things which really made a huge difference to practice?
A: Well, the management of minimal change with steroids made a big difference. Sorting out of the aluminium situation, which was really Robin’s thing. The introduction of more liberal diets made quite a difference.
N: What led to that?
A: Well, as far as acute renal failure was concerned, it was the ability to do more frequent dialysis so that you were keeping the blood urea and creatinine at reasonable levels. I suppose the same was true in chronic renal failure. That certainly was a help.
- Peritoneal dialysis
- Undergraduate teaching
- Looking back on the route taken, and some professional advice
N: Anne we haven’t talked very much yet about peritoneal dialysis, which I think, was first used in various places for acute renal failure.
A: We introduced peritoneal dialysis for acute renal failure in people whose circulation was sufficiently unstable to make us a little unwilling to put them on haemodialysis. And also, for people who came in with an emergency in the middle of the night and we persuaded ourselves that it was safer to do a peritoneal dialysis than to start setting up for haemodialysis.
N: Where did you get the recipes for peritoneal dialysis? Or the methodology?
A: Do you know, I don’t know. The fluid was available commercially. I don’t know who had done it before we did.
N: Do you remember the first patient you treated this way?
A: No, not clearly.
N: And when would it be do you think? So, haemodialysis was 1959.
A: It would be in the 1960s probably in the late 1960s.
N: So I think other places, perhaps places without haemodialysis machines, might have been earlier than that?
A: I think so.
N: And what was experience like with it?
A: Very good for a single acute peritoneal dialysis or even for a week or so, preparing new dialysis for acute renal failure. Like everyone else when we started doing it in chronics we got patients getting infection – blocked cannulae and fibrosing peritoneum.
N: Yes, indeed. And you must have been, because I think there were only for a while there were only two centres in Scotland doing haemodialysis, you must have been sent patients from remote locations occasionally?
A: Yes, in the first year or so we got patients from Stornoway and various other distant places. By the end of … when we started there was a unit which started about the same time at Glasgow Western. And shortly afterwards, Glasgow Royal started and then Dundee started a bit later. But we certainly got patients from a distance. They usually arrived pretty sick. But usually because they were uraemic in that there been a delay in referring them, rather than shocked because as I said earlier, the shock patients didn’t survive long enough.
N: Had many of them had peritoneal dialysis before they came?
A: I don’t think any of them had
N: Shall we move on to later on in your career when I know you began to get involved in teaching increasingly, or maybe you did some of that from the beginning?
A: I read my own account of things. I did get involved in the beginning. As an SHO I was giving clinical teaching. As a young lecturer, I was responsible for the final year students in the ward.
As a young lecturer, I also was responsible for the water and electrolyte lectures in the therapeutics course. And various other ones. Because one of the less likeable things about Sir Derrick was that he was apt to telephone from London to his Secretary and say, ‘Get one of the chaps or Miss Lambie to give my therapeutics lecture. It’s on acute leukaemia’. And that was one, there were various others. That was the one time we all said, ‘No, we’re not going to talk about something we know nothing about’. But he had this idea that it didn’t do us any harm, to be asked at short notice to lecture on any subject.
N: A useful skill.
A: Any lecture of any importance is rehearsed. My Honyman Gillespie lecture was rehearsed twice as far as I remember before he was satisfied.
N: What was your Honyman Gillespie lecture about?
A: Potassium excretion. It wasn’t a terribly good lecture because one couldn’t use animal data. It was very difficult. But I had done a good deal of teaching on the wards and quite a bit of lecturing most of my career.
N: And then, I think, probably relatively late in your career, there was talk about reforming the curriculum.
A: Yes, I got involved in the committee for the first two years. And specifically, was told I was doing the clinical correlation course. That would be about maybe 1984-85. That came as a bit of a shock because I never really had any serious thoughts about that. Being a conventional sort of person I was really quite happy with the teaching we were doing. I had quite a struggle persuading consultants in a variety of specialties to set aside time to teach first year students. They felt that it was a waste of their time.
N: So this was clinicians lecturing at a time point, when historically these would have been very science-based lectures with pathology as the sole clinical correlation probably, Is that right?
A: While we ran it, to begin with they had problem-based projects and then they came once a week and had either a clinical lecture (which I did several myself, because it was difficult to get people to do them) where patients were demonstrated. And one tried to make them use (it was a question and answer to the whole class), one tried to make them use their knowledge of basic sciences to sort out what might be wrong with the patient. And they were popular actually and worked out quite well. I also tried to arrange visits to a number of units. And that’s when I ran into difficulty. People felt that with having the clinical students in the wards they’d got enough.
N: You mentioned problem-based learning. What was that like?
A: It went very well, actually.
N: Were you involved in designing this or just delivering it?
A: I was involved in designing it to the extent that I said, we will find so many clinicians who will be prepared to have a group of students studying something. An example was that the professor of anaesthetics very kindly took a group and got them to test mental acuity at short intervals following general anaesthetics, which was an interesting one. And we, the problem based, like learning projects, had to be split between the clinical people in the Royal and the Western and the psychology people. That was the condition of which they gave up some of their lecture time. So they organised some projects, and clinical people organised some projects. And then at the end of the autumn term, there were four nights set aside when they met at the headquarters of the Royal Medical Society. And the papers were delivered and there was coffee and buns and general discussion. And there was, as far as I remember a prize for the best, and that they were quite popular.
N: So that did sound like the wind of change for the curriculum, which I think has been through another couple of rounds since then. But it was probably the beginning.
It’s fascinating to look back on a career … is there anything that you wish had gone very differently or that you’re just hugely, feel hugely privileged to have been a part of?
A: I feel that I was very privileged. I feel that I was very lucky as a girl to get on the ladder in a teaching hospital. I feel that I was lucky, having clinical work to which I could apply my limited knowledge of basic sciences.
I’ve enjoyed working as a member of a team. And incidentally, the first experience I had of that was when we started acute renal failure, because particularly in the early dialysis, it involved a big team of people: two physicians, a surgeon, a haematologist, someone from clinical chemistry, very often a bacteriologist. And it was probably the first time a team of that sort had worked together in the Royal Infirmary.
N: That’s pretty amazing to reflect back on. And it was the height of technology at the time. Perhaps before then …
A: Oh, I’d forgotten the medical physicist!
N: Some people’s accounts of that period describe the increasing responsibility placed on these other members of staff as the service got bedded in, and I’m sure you must have seen that too. You mentioned earlier how dialysis became a nurse provided service.
A: It certainly took more time. In the early days of dialysis, I still did quite a bit of endocrinology, and a good deal more general medicine. And more research. And that did get crowded out, all these things were curtailed a bit. In some way, some of the pleasantest years were the two three years after I came home, and before the establishment of dialysis when life was a little more leisurely and the Renal Association to which we belonged was more academic, with a mixture of clinicians who were interested in research and a lot of pure scientists. And there was time for more thought and discussion. And gradually, that was eroded.
N: It became service-driven.
A: Yes.
N: Do you think you made the right career moves?
A: Yes. Yes, I do. (are we recording? You can eliminate things?!) Shortly before I went to the States, Michael Oliver gave me a lift home, and was asking me what I was proposing to do. And I said I was getting interested in potassium and acid base balance. This was even before I went to America. And he said, ‘Well, I think the important thing as a girl is that you should have a wee racket’ And I said, ‘by which you mean?’ and he said, ‘something that practically nobody else is interested in’. It was very good advice.
N: I’m not sure that’s unique advice to girls though (laughing)
A: Yes, that probably applies to everyone.
N: But your interest actually then turned out to be the foundations of a huge specialty. So that scotched that plan!
A: Well, that was very fortunate.
N: OK shall we stop? Anne, thank you very much indeed
A: I hope it’s accurate, I think most of it is.
Authorship
Neil Turner, with thanks to John Feehally for additional work on the transcript. The interview was facilitated by Kidney Research UK.
Last Updated on June 26, 2023 by neilturn